Share your perspective and help improve the health of our community! We are conducting a Community Health Needs Assessment (CHNA) to help us better understand the health needs of the community our health system serves. Learn more and take the short survey.
Lyme Disease and Post-Lyme Syndrome
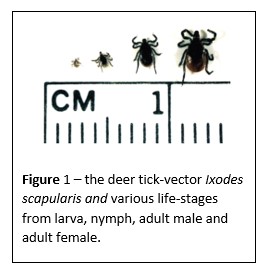
Lyme disease is commonly included in our differential diagnoses of annular appearing rashes and often alluded to as a potential source for chronic fatigue syndromes. In this article we review a general approach to the evaluation for Lyme infections. Lyme disease is a tick-borne illness, which is caused by the pathogenic species of the spirochete Borrelia. The Ixodes tick-vector (Figure 1) and Borrelia species are endemic to the US between April and September in the Northeast, Middle Atlantic and North Central states.
The clinical manifestations of Lyme disease can generally be divided into three phases: early localized, early disseminated, and late disease.
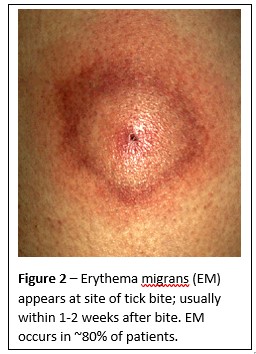
Early-Localized Disease is characterized by an erythema migrans (Figure 2) rash in 80% of cases and it’s associated symptoms may include: fatigue, malaise, lethargy, mild headache, mild neck stiffness, myalgias, arthralgias or regional lymphadenopathy.
Early-Disseminated Disease generally occurs weeks to months after a tick bite and although rare, may include: carditis, neurologic disease, migratory arthralgias, multiple EM skin lesions, lymphadenopathy, ocular involvement, liver disease and renal toxicity.
Late or Chronic Disease (Post-Lyme Syndrome) is described as occurring months to years after a tick bite and is exceedingly rare. Clinical manifestations are proposed to include arthralgias, neurologic disease and chronic cutaneous changes.
A diagnosis of Early-Localized Lyme disease is based primarily on a clinical history when the characteristic EM lesion is present in a patient who lives in or has recently traveled to an endemic area and reports a high risk for tick exposure or history of removing a tick after an extended blood meal.
In later stages of Lyme disease, the patient should again meet the criteria for an Early-Localized Lyme infection in their clinical history and serological testing for antibodies to B. burgdorferi can be performed as an adjunct to the clinical diagnosis. By itself, serologic testing can neither establish nor exclude the diagnosis of Lyme disease.
When testing is warranted we use a two-tiered approach:
- First Tier: EIA, ELISA or IFA which measures overall antibody response (IgM and IgG to Borellia antigens). These screening tests are very sensitive but not specific to disseminated disease. If equivocal or positive, a confirmatory test should be performed (second tier).
- Second Tier: Western immunoblot detecting antibodies to preselected Borellia antigens. This test is very sensitive and specific for disseminated Lyme disease but both tiered tests should be positive for late stage disease.
Lyme disease serologic testing should not be performed on asymptomatic patients or evaluation of patients who present with nonspecific symptoms such as fatigue, myalgias or arthralgias. We do not test these patients since the use of serologic testing in populations with a low pre-test probability of Lyme disease results in a greater likelihood of false-positive test results.
In patients with noninflammatory musculoskeletal pain, cognitive complaints, fatigue, and/or irritability, alternative diagnoses should be considered, such as chronic fatigue syndrome, fibromyalgia, myofascial pain syndrome, polymyalgia rheumatica, hypothyroidism, inflammatory myopathies, and chronic traumatic encephalopathy.
Finally, in cases where early Lyme disease is strongly suspected, the preferred treatment regimens include:
1. Doxycycline 100 mg PO bid for 14-21 days
2. Amoxicillin 500 mg PO tid for 14-21 days
3. Azithromycin 500 mg PO daily for 7-10 days
In the case of Post-Lyme Syndrome we do not recommend antibiotic treatment. In prospective blinded placebo-controlled trials, there has been no benefit related to antibiotic therapy.3 Furthermore, there is a risk for patient harm directly related to drug interactions or IV catheter associated complications (bacteremia, thromboembolism).
When to refer to the Infectious Disease Clinic
The Infectious Disease team can assist in outlining medical management in cases where there is a strong suspicion of Lyme Disease and the patient meets criteria of a known tick exposure and the characteristic erythema migrans.
References:
1) IDSA Guidelines: Clinical Infectious Diseases. 43:1089, 2006
2)New Eng J Med. 370:1724, 2014
3) New Eng J Med. 374: 1209, 2016
4) JAMA 315:1767, 2016
5) Images from UpToDate

