Measles Exposure Notice: We’re responding to a confirmed case of measles at Valley Medical Center’s Emergency Department on Sunday, Oct. 26. We’re working closely with public health to notify anyone who may have been exposed. Learn more.
Healthcare is on the ballot this November. Learn about Hospital Prop 1.
Your Partner in Fighting Cancer
Building relationships is a priority for us. With the latest treatments available in your backyard, living with cancer doesn’t have to mean living in a hospital or traveling long distances for care. We are proud to have exceptional doctors and treatment options close to home so our patients and their loved ones can make the most of every single day.
A Multidisciplinary Approach to Cancer Treatment
Caring for our community like family is our priority at Valley and we are proud to provide outstanding clinical cancer care and leading-edge treatment options for our neighbors – close to home. We place an emphasis on prevention, early detection, improved outcomes, reduced side effects and less invasive treatment options. We deliver innovative care and therapies with patient-focused support and guidance.
Physicians specializing in medical oncology, radiation oncology, neuro oncology and surgical oncology as well as specially trained nurses and technicians, social workers, physical therapists and nutritionists provide support through each stage of your care. Your multidisciplinary team of board-certified specialists gather regularly to review your case. Should you need more advanced care for a rare or complex diagnosis, we closely consult and coordinate care with renowned local resources.
A Focus on Healing
Designed to enhance comfort and dignity for our patients, our healing environment incorporates restorative natural elements like sunlight and water. Valley Medical Center is also proud to offer a Healing Garden and Serenity Garden, as well as an Inpatient Family Retreat, to provide peace and respite for patients and loved ones.
We also partner with Cancer Lifeline for classes and support groups to help you and your loved ones build strength and understanding, reduce stress and find comfort with others who understand your journey.

Valley Medical Center is accredited with Commendation by the Commission on Cancer as a Community Hospital Comprehensive Cancer Program. Learn more.
Cancer Care
The physicians at the Oncology & Hematology Clinic diagnose, evaluate and provide treatment strategies for patients with cancer and disorders of the blood and bone marrow. Our medical oncologists work to provide best-in-class care and treatment for patients with cancer and work collaboratively to ensure a comprehensive approach to treatment for each patient.
Oncology and Hematology Services
Treating cancer is a collaborative endeavor. Our medical oncologists work closely with surgeons, radiation oncologists, infusion teams and other specialists to help patients understand their diagnosis, create individualized treatment plans, and coordinate and provide effective treatment for patients with:
- All types of cancer
- Blood-related disorders
- Bleeding and coagulation disorders
- Blood and marrow disorders, including leukemia, lymphoma and multiple myeloma
Blood and Marrow Disorders
The Oncology and Hematology Clinic is staffed by skilled, experienced medical oncologists and hematologists with expertise in treating:
- Iron deficient anemia
- Sickle cell anemia
- Hemoglobinopathy
- Myeloproliferative disorders
- Myelodysplasia
- Idiopathic Thrombocypenia
Our Physicians
Each Oncology and Hematology physician is board-certified in medical oncology. As a team, they bring extensive experience in research and academic training at distinguished centers including the Mayo Clinic, Yale University, University of Southern California, University of Washington/Fred Hutchinson Cancer Research Center and Seattle Cancer Care Alliance. Several have served as leadership for national and state medical oncology organizations and publish in medical journals. Most importantly, they provide outstanding, compassionate care.
Types of Treatment
- Chemotherapy - Treating cancer with drugs.
- Hormone therapy - Using hormones as treatment for prostate and breast cancers.
- Biological response modifiers - Using special compounds to fight cancer by stimulating the body's immune system
The Breast Center
Working with The Breast Center, Valley Medical Center’s state-of-the art breast screening and diagnostic center, we diagnose and evaluate patients whose mammograms have resulted in abnormal findings and treat patients who have been diagnosed with all types and stages of breast cancer.
Infusion and Immunotherapy Center
Oncology and Hematology physicians collaborate closely with Valley Medical Center’s Infusion and Immunotherapy Center to treat cancer in a way that successfully brings about remission or prolongs life, while maintaining good quality of life. Therapy programs vary according to each patient’s needs.
Radiation Oncology
Valley Medical Center's Radiation Oncology provides patients sophisticated, close-to-home radiation therapy treatment.
Gynecologic Oncology is a medical specialty that offers an integrated approach to the diagnosis and surgery of cancerous and precancerous conditions of the female reproductive system. These include cervical dysplasia and cancer (abnormal Paps smears), ovarian cancer, pelvic masses, postmenopausal bleeding and uterine cancer (uterine sarcoma and endometrial cancer), vaginal cancer and vulvar cancer and hereditary cancer syndromes.
At Valley Medical Center, our gynecologic oncology team will provide you with patient-centered cancer treatment. A gynecologic oncologist, doctor with specialized training in treating gynecologic cancers, will oversee your care from diagnosis to completion of treatment. Our gynecologic oncologists serve as both surgeons and medical oncologists (chemotherapy treatment).
In addition to a gynecologic oncologist, you will have other expert providers making up your treatment team depending on your personalized needs for surgery, chemotherapy, and/or radiation. This may include a radiation oncologist, oncology nurse navigator, research nurse, and genetic counselor.
To learn more, click here.
Your entire breast cancer care team, in one visit, to create a personal care plan for you.
Our breast multidisciplinary clinic (MDC) offers a comprehensive clinic visit with a breast surgeon, radiation oncologist and medical oncologist in one day. This team of healthcare professionals works in collaboration with you to develop a personalized plan of care using nationally-recognized best practice guidelines. A process that might otherwise involve multiple visits is completed in a single day allowing for a more timely start of treatment and providing comprehensive cancer care to you and your family.
Your day at MDC begins with a visit and exam with a breast surgeon. Next, your care will be discussed in a tumor board by our entire team of specialists who will develop your individualized treatment plan. You will then have an opportunity to meet independently with the breast surgeon, radiation oncologist, and medical oncologist to review your results, the recommended treatment options, answer questions, and discuss the next steps. By the conclusion of the MDC visit, you will take home an individualized plan of care.
Our Nurse Navigators will partner with you and your family to offer support, answer questions, assist with scheduling appointments, and coordinating care throughout your cancer journey. Additional resources are available to you and your family through our cancer support services to address any barriers to care, psychosocial and financial support.
Your Breast Cancer Care Team Includes:
| Medical Oncologist | Radiation Oncologist |
| Breast Surgeon | Breast Radiologist |
| Pathologist | Genetic Counselor |
| Social Worker | Lymphedema Specialist |
| Supportive & Palliative Care | Financial Advocates |
| Oncology Nurse Navigator |
VMC’s robotic surgery option provides a less invasive cancer surgery alternative with faster recovery times and fewer side effects.
Physicians at Valley Medical Center's Neuroscience Institute treat patients with benign or cancerous tumors of the brain, spinal cord and nerves. Benign nervous system tumors, while not cancerous, may require ongoing treatment.
Learn more about Neuro Oncology.
If you're thinking about genetic testing because cancer runs in your family, or you've had it yourself, you might find it especially important if you or a relative had:
- Breast cancer before age 50
- Ovarian cancer at any age
- Colon cancer before age 50
- Endometrial cancer before age 50
- Metastatic prostate cancer
- Pancreatic cancer
When you first visit us, we'll talk about your health history and your family's. We'll help you understand your own risk of cancer, and we'll go over the benefits and limitations of genetic testing so you can decide if it's right for you. If you have a higher risk of breast cancer, we'll stay in close touch to manage your screenings. If you decide to go ahead with genetic testing the process is simple—it's just a blood test or saliva sample.
Insurance usually covers the cost of consult appointments with genetic counselors. If you have concerns about your insurance plan coverage, we're here to help with all the insurance details before you come in. For patients who choose to go ahead with genetic testing and pay out-of-pocket, it generally costs less than $100.
Click here to view clinic information.
From spacious rooms where family or friends are welcome, to free WiFi, warm blankets, room service and bedside entertainment, it is our goal to provide a healing and relaxing environment. Located on the main floor of Valley Medical Center (3B), the Infusion & Immunotherapy Center offers a wide variety of treatments for cancer.
Click here to learn more.
Our team of radiation oncologists and therapy staff take a holistic approach and are dedicated to providing support and comfort throughout the course of radiation therapy. We offer advanced technologies for the following modalities:
- Intensity Modulated Radiation Therapy (IMRT)
- Volumetric Modulated Arc Therapy (VMAT)
- Image Guided Radiation Therapy (IGRT)
- Stereotactic Radiosurgery (SRS)
- Stereotactic Body Radiotherapy (SBRT)
- Customized treatment plans utilizing Monte Carlo algorithms
- High Dose Rate Brachytherapy for Breast and Gynecological cancers (SAVI, Tandem & Ring, Cylinder)
- Low Dose Rate Brachytherapy Prostate Seed Implants (Pd-103 and I-125)
Learn more about Radiation Oncology.
Comprehensive, Advanced Breast Cancer Care in Your Community
With the latest treatment available in your backyard, living with cancer doesn’t have to mean living in a hospital or traveling long distances for care. We are proud to have the right doctors and treatment options close to home so our patients and their loved ones can make the most of every single day. Learn about breast cancer care at Valley.
Cancer Prevention & Education
The earlier cancer is detected, often the easier it can be to treat and cure. Therefore, early detection is key to improving survival for patients diagnosed with cancer. Valley Medical Center offers the latest technology that help detect cancer and save lives:
- Biopsy & needle localization
- Diagnostic imaging (MRI, CT, PET Scan, Nuclear Medicine)
- Digital mammography
- Endoscopy & colonoscopy
- General diagnostic radiology
- Gynecologic oncology
- Laboratory testing
- Pelvic exam and pap test
- Surgical assessment & staging
- Ultrasound
When to Get a Colorectal Cancer Check
Age 45 or older?
|
Excluding skin cancer, colorectal cancer is the third most common type of cancer in both men and women the United States. It strikes more than 140,000 Americans and kills about 50,000 every year. It's one of the most curable cancers if detected early, but it often produces no symptoms until it's beyond successful treatment. It is thought that most colon cancers develop when environmental factors interact with a person’s inherited or acquired susceptibility. Most colon cancers come from a type of growth in the large intestine called an adenomatous polyp. These polyps can slowly change, usually taking many years to develop into cancer.
That's why everyone should be aware what risk group he or she falls into and when to begin screening for colorectal cancer. Valley Medical Center makes scheduling easy with Direct Access. Learn more.
All women and men at average risk for colorectal cancer should have a screening test for colorectal cancer beginning at age 45 (colorectal cancer is rarely found in people under the age of 45).
People who are at higher risk for colorectal cancer may need to begin screening tests at a younger age.
People at higher risk include:
- Those with familial polyposis; that is, a family history of development of multiple polyps likely to become cancerous. Although only about 1 percent of all colorectal cancer patients have this gene, those who do have it have a nearly 100 percent chance of developing cancer. People with this cancer will likely die in their 40s if not treated. They should start screening in their teenage years.
- Those with hereditary non-polyposis cancer (HNPCC, also known and Lynch syndrome), which is brought about by defective DNA repair genes. About three to five percent of people with colon cancer have this condition. People with HNPCC typically have parents or siblings who developed colorectal cancer before age 50. They should start screening in their 20s, or about 10 years before the youngest age of the family member who developed colorectal cancer.
- Those who have had colorectal cancer or a precancerous polyp.
- Those who have a parent, sibling, or child who has had colorectal cancer before the age of 60, or if more than one relative is affected (at any age), have a two to four times greater risk.
- Those who have chronic inflammatory bowel disease (ulcerative colitis or Crohn's colitis), a condition that causes the colon to be chronically inflamed, have an increased risk of developing colon cancer. Screening should be started at a young age and be done more frequently.
Several methods can be used for screening. A person’s preference and the recommendation of his or her healthcare provider should determine which test is used and how frequently a person is screened.
- The fecal occult blood test (FOBT) and fecal immunochemical test (FIT) look for hidden (occult) blood in stool. Blood in the stool can be caused by a variety of conditions; colorectal cancer is only one of them. The FOBT uses a chemical reaction to detect blood in small samples of stool that have been placed on a FOBT sample card. Usually two samples from each of three consecutive stools are collected at home and mailed or taken to your health care provider’s office for testing. Certain foods or drugs can affect the FOBT, so you should follow instructions on diet and medications.
- The FIT looks for a specific part of a human blood protein. Collecting samples for the FIT is easier (there are no drug or dietary restrictions during testing), but the test is more expensive than the FOBT. The American Gastroenterological Association (AGA) and the American Cancer Society (ACS) say that if a test is positive for blood in stool, a colonoscopy should be done to determine the source of the bleeding. It could be caused by cancer, a polyp, hemorrhoids, diverticulosis (a condition in which small pouches form at weak spots in the wall of the colon), or inflammatory bowel disease (also called colitis). If cancer or a precancerous polyp does not bleed, this test will not detect it. For people at average risk who choose this test, the ACS and the AGA recommend that it be done once a year.
- Sigmoidoscopy uses a short, flexible, lighted tube tube that is inserted into the rectum and gently moved into the lower part of the colon. It is a common screening method, but only covers the lower part of the colon, representing less than half the surface at risk for developing cancer. Before this test is done, the colon and rectum must be cleaned with an enema. The ACS recommends that people at average risk have it done every five years.
- Colonoscopy uses a colonoscope, a slender, flexible lighted tube that is longer than the one used for sigmoidoscopy. In a colonoscopy, the entire colon is examined. If a polyp is found, it can be removed during the colonoscopy. Before a colonoscopy, the entire colon must be cleaned with laxatives and/or enemas. A colonoscopy can be uncomfortable, so an intravenous medication is usually used to make you feel sleepy during the procedure. Colonoscopy takes about 30 minutes, longer if a polyp is removed. A colonoscopy is recommended every 10 years.
- Double-contrast barium enema (DCBE) is a type of X-ray test. Barium sulfate, a chalky liquid, and air are used to outline the inner part of the colon and rectum to look for abnormal areas on X-rays. If suspicious areas are seen on this test, a colonoscopy will be needed to explore them further. This test is recommended every five years.
Newer methods of screening for colorectal cancer may be recommended as screening options.
- Virtual colonoscopy (also known as CT colonography) is a three-dimensional CT scan of the colon. Some people may prefer it to a standard colonoscopy because it is not as invasive, although it still requires that the entire colon be cleaned with laxatives and/or enemas beforehand. If polyps are seen in a virtual colonoscopy, a standard colonoscopy will need to be done to remove them. This test should be done every five years.
- Stool DNA tests look for certain abnormal sections of genetic material from cancer or polyp cells in the stool. These tests are not invasive and don't require any special preparation, but they are expensive. An entire stool sample is collected at home and mailed to a lab for processing. People having this test will receive a kit with detailed instructions from their doctor's office or clinic on how to collect the specimen. As with other stool tests, if the results are positive, a colonoscopy is needed to investigate further. Because this is a newer type of test, the best length of time to go between tests is not yet clear.
Screening for those at higher risk
The ACS makes the following recommendations:
- If you have had a precancerous polyp or colorectal cancer, you should follow the recommendations of your healthcare provider.
- If you have a parent or sibling who had colorectal cancer before the age of 60, or two or more close relatives who had colorectal cancer at any age, you should have a colonoscopy beginning at age 40, or 10 years before the youngest case in the immediate family. Screening by colonoscopy should continue every five years as long as the results do not show a precancerous polyp or cancer.
- If you have a family history of familial adenomatous polyposis (FAP), you should be under the care of a specialist, and you generally should begin screenings at puberty.
- If you have a family history of hereditary non-polyposis colorectal cancer (HNPCC), you should be under the care of a specialist, and you generally should begin screening in your early 20s, or 10 years before the youngest case in your immediate family.
- If you have inflammatory bowel disease (chronic ulcerative colitis or Crohn's disease), you should be under the care of a specialist who can determine when screening should begin.
The prostate is a gland that wraps around a man's urethra, the tube that carries urine from the bladder. Cancer can form inside this gland and exist for years without causing symptoms.
If you are a man, you are at risk for prostate cancer. The risk for prostate cancer increases with age. Your risk is also higher if you are African-American or have a family history of prostate cancer. The American Cancer Society recommends that men over age 50 get tested for prostate cancer once a year.
Learn about screening for prostate cancer.
Regular screening mammography can often detect breast cancer long before it can be felt.
Valley's Breast Center is an outpatient breast imaging center that offers screening and diagnostic mammography, breast ultrasound, breast biopsy and bone density screening.
Click here to learn more about the Breast Center.
 Every woman is at risk for breast cancer. One in eight will develop the disease, and 85% of those who are diagnosed have no family history of breast cancer. This is why experts at Valley's Breast Center believe that mammography remains the most effective tool for the detection of breast cancer at its earliest and most treatable stages.
Every woman is at risk for breast cancer. One in eight will develop the disease, and 85% of those who are diagnosed have no family history of breast cancer. This is why experts at Valley's Breast Center believe that mammography remains the most effective tool for the detection of breast cancer at its earliest and most treatable stages.
A mammogram is a low-dose x-ray that allows radiologists to look for changes in breast tissue. The Breast Center is proud to provide patients 3D mammography combined with 2D mammography as our standard of care.
The American College of Radiology, Society of Breast Imaging, National Comprehensive Cancer Network, and American Society of Breast Surgeons recommend annual mammography screening starting at age 40 for average risk women. In fact, with early detection, the average five-year survival rate for breast cancer is close to 99%.
Types of Screening
- Mammography
- Breast MRI
- Breast Ultrasound
Make breast health a priority in your life—do your monthly self-checks and schedule your annual mammogram today with The Breast Center in Renton or Covington.
 Directly schedule your mammogram in MyChart.
Directly schedule your mammogram in MyChart.
( What is MyChart?)
The Breast Center at Valley Medical Center follows strict federal guidelines to ensure mammography equipment is safe. The lowest doses of radiation are used, while capturing the breast tissue images more clearly in three dimensions.
Clinical Pharmacy
In conjunction with the medical staff, clinical pharmacists provide intravenous nutritional support and pain management for patients in the hospital. In coordination with medical oncologists, the IV therapy team, oncology nurses and clinical pharmacy staff, VMC provides patients with a full range of intravenous and transfusion therapies, as well as supplies and infusion pumps, 24 hours a day.
Rehabilitation
Rehabilitation is available to inpatient and outpatient cancer patients through Occupational, Physical, Speech, and the Lymphedema Management program. The goal of Rehabilitation Services is to maintain or increase a patient's ability to remain independent in self-care, mobility and communication for as long as possible. The department helps with discharge planning to ensure a safe return home, with appropriate resources, and to teach family members how to provide appropriate assistance to the patient.
Enterostomal Therapy
Education and support are provided to individuals who have undergone bowel or bladder surgery that results in changes in elimination, as well as to individuals who have draining wounds, pressure sores and other skin problems requiring ongoing management.
Nutritional Guidance
A dietitian is available to provide counseling regarding dietary problems related to cancer and cancer treatment. Services are provided at VMC's Diabetes Education & Nutrition Clinic in Kent.
Home Health Agencies
Healthcare support services are offered to oncology patients in their homes upon recommendation of and under the guidance of the patient's physician. Home care services are administered by an interdisciplinary team that includes nurses, physical therapists, speech therapists, social workers, home health aides and enterostomy therapists. Services can be provided on an intermittent home visit basis or hourly. The home care team provides information and instruction to help the family or caregiver manage pain, disease symptoms and treatment side effects. The goal of home care is to return the patient to the highest level of functioning, or to make the patient as comfortable as possible through the end of life.
Lymphedema Management For Patients Following Breast Cancer Treatment
The Rehabilitation team at Valley Medical Center would like to help you recover faster, and be able to return to your normal activities following your treatment for breast cancer. Please review the Activity Guidelines and Exercises After Breast Cancer Surgery flyer to help your recovery. Please let your healthcare provider know if you are experiencing any of these symptoms beyond the normal post- operative period for healing (usually six weeks):
- Pain in your chest or arm
- Limited arm or trunk motion
- Inability to perform normal daily functions
- Excessive fatigue
- Significant swelling of your arm, trunk, or breast
Your healthcare provider will help you determine if these symptoms are part of your normal healing process, or if you would benefit from the additional help from our rehabilitation team. A customized program will be developed for you, and may include any or all of the following:
- Range of motion exercises, particularly for trunk and shoulder
- Postural training
- Gradual strengthening and conditioning exercises
- Scar management
- Pain and symptom management
- Swelling management (see below)
- Education about continued self care
In particular, if you notice swelling that persists in your arm or chest, your healthcare provider needs to evaluate if you may have early signs of lymphedema. This condition can occur following lymph node surgery or radiation therapy. Symptoms of lymphedema include:
- Swelling of the arm or trunk
- Feeling of heaviness of the arm
- Achiness or pain
- Tight clothing or jewelry
Valley Medical Center offers highly specialized treatment for lymphedema called Complex Decongestive Therapy. This internationally endorsed approach consists of four parts:
- Patient and family education for prevention and self-management
- Manual lymph drainage to stimulate lymph flow through specialized massage
- Compression with bandaging, garments, and occasionally mechanical pumps
- Active exercises to help mobilize fluid and assist motion
Skilled therapists who have been certified by a 175-hour training course provide this specialized care. They will design a program to meet your needs, whether it’s for early management and education or intensive daily therapy. Valley Medical Center is a National Lymphedema Network sponsored treatment center.
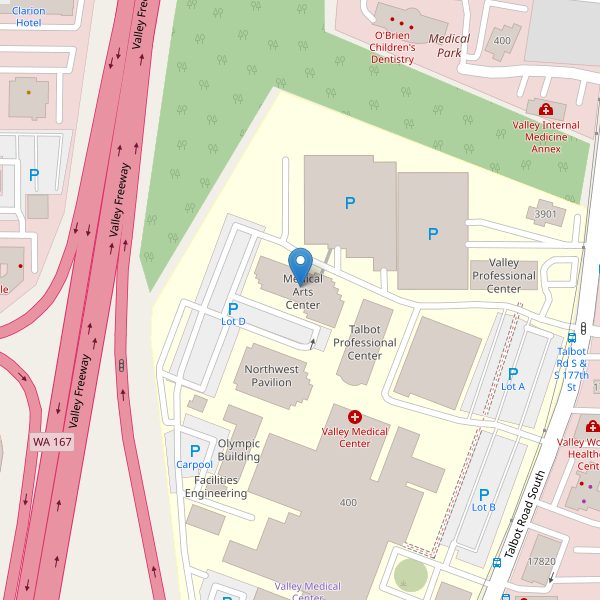
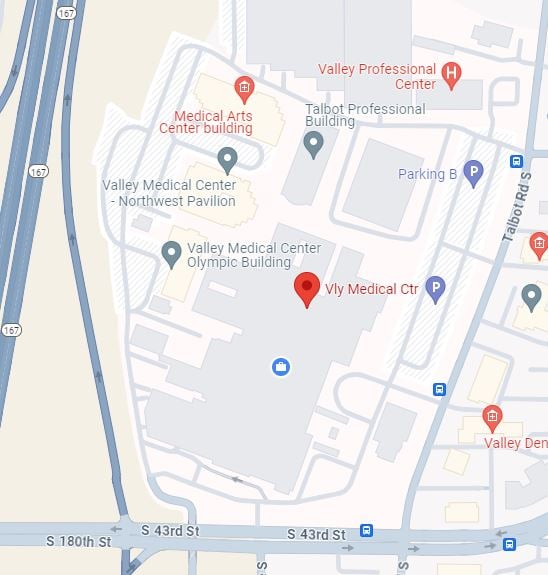
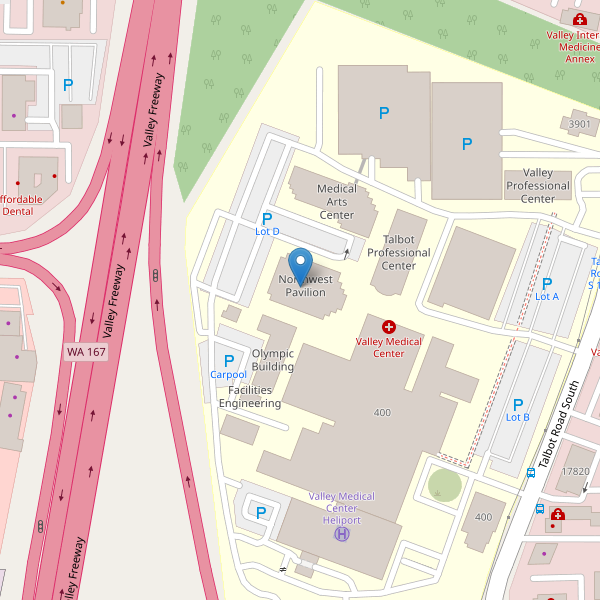
To Make an Appointment
A referral from your healthcare provider is needed for treatment and payment by your insurance. Talk about your concerns with your provider and ask for a therapy referral. The Rehabilitation Department is located in the Northwest Pavilion of the hospital. To schedule an appointment, call 425-690-3650.
Patient & Caregiver Resources
As you begin your cancer care journey, we strongly encourage you to take time for you. Physically. Mentally. Emotionally. After all...your healing is all about YOU. You have not “become” your illness.
It may surprise you that people often express a sense of loss during short or long medical procedures—not physical so much as personal. Medical needs can overwhelm us and impact our outlook on life and how we cope with life’s challenges. This is normal.
Medical needs can lead you to think “I don’t know myself anymore” or that “I’ve lost a part of me.” Don't worry. Just know it's more misplaced than lost. You'll come to experience many feelings. This is very common, even expected.
At Valley, we walk beside you on this journey. No doubt, treatment rooms and medical procedures will strike you at first as unfamiliar ground. We encourage you to think of them as safe ground—safe for your body, mind and spirit. Behind every machine, therapy, surgery or paperwork is a staff member ready to help guide and support you.
These resources can help you learn how to live your best life with cancer:
Welcome your support network of friends and loved ones to join you on the journey. When going through infusions, chemotherapy, radiation treatments or other medical procedures, there is a tendency to feel alone. It helps to connect to your resources outside the hospital or clinic.
Remember: your family and friends understand you best. They may not understand all your medical care—but they don’t have to be medical professionals in order to support you. Let them be there for you to provide comfort, companionship, diversion and yes, even humor.
People close to you often want to help but may not know how. Let them be part of your medical journey. Share how you're feeling and how they can help lighten your load.
At times, it will be beneficial for you to let go of what you cannot change. A good question to ask is “How am I going to handle this?” You may need to find some energy, resources and support. Let your support from loved ones, community, support groups, faith-based organizations or other associations be a part of your cancer care journey.
There are also some helpful tools and practices you may want to consider to help you cope by finding moments of solitude, reflection, inspiration and hope:
- Healthy “non-medical” practices like tai chi
- Find comfort and solace in nature, learn about the art of "forest bathing"
- Deep reflection, contemplation, meditation
- Read or listen to inspirational writings or poetry
- Try some of your own creative writing or keep a personal journal
- Listen to music, old and new
An oncology social worker is available to assist you and your loved ones in addressing the new and complex challenges a diagnosis of cancer can bring. Our oncology social worker is a licensed, master’s level social worker with specialized training and experience in assisting people impacted by cancer. Services are available throughout all phases of your cancer care from diagnosis, through treatment and into recovery.
These services are offered at no additional cost as they are considered an important part of your total medical care:
- Access information so you can understand your diagnosis and treatment plan.
- Cope with your cancer diagnosis and the different emotions you may experience while dealing with cancer and its treatment.
- Consider decisions about treatment options in light of other factors in your life, including work, family, personal goals, needs and responsibilities.
- Understand and complete durable power of attorney (DPOA) and advanced directives.
- Understand social security, disability benefits and medical insurance.
- Get information about, and apply for, programs and services in your local community and nationally that may be able to help during this time.
The oncology social worker can offer you:
- Counseling for you and your loved ones, to address issues related to your cancer diagnosis and deal with things such as depression, anxiety, stress, the effects of cancer on the family and relationships, etc.
- Referrals to community-based counseling as needed.- Support groups and educational programs for you and your caregivers.
- Support, education and referrals for parents or caregivers of minor children regarding how to best support children when a loved one has cancer.
- Information about and referrals to community resources for help with financial concerns, housing concerns, food assistance, transportation issues, etc.
- Information about, and referral to, cancer-related information and service organizations.
- Resources and education related to workplace issues and schooling.
- Resources to help you cope with common treatment side effects.
The oncology social worker can teach you about:
- Talking effectively with your treatment team members to get the care you want.
- Talking with your children, family, friends and co-workers about your cancer diagnosis and treatments.
- Coping with your emotions, such as sadness, anger, grief, and worry or fear.
- Reducing stress and using relaxation skills, such as guided imagery, progressive muscle relaxation, etc.
- How cancer can affect sexuality, intimacy, fertility, and general feelings about your body and appearance.
- Living with cancer; issues commonly experienced and resources to help you.
- Planning for your care with the use of advance directives.
- Dealing with transitions during and after treatment and life as a cancer survivor.
The oncology social worker can help you access:
- Affordable medical care and prescription drug coverage
- Prescription drug assistance programs
- Financial assistance programs and help with daily living needs
- Transportation to and from medical care
- Referrals for help at home, home health care and hospice care
To learn more about Cancer Support Services, please call 425.690.3507
American Cancer Society
American Cancer Society Online Resources
1.800.237.2345
A nationwide, community-based volunteer health organization dedicated to eliminating cancer as a major health problem by preventing cancer, saving lives, and diminishing suffering from cancer, through research, education, advocacy, and service.
CancerCare
CancerCare Online Resources
CancerCare is a national organization committed to helping people cope with the emotional, practical and financial challenges of cancer. CancerCare’s comprehensive network of services includes telephone, online and in-person counseling and support groups, education, publications, resources and financial and co-payment assistance. All CancerCare services are provided by professional oncology social workers and are completely free of charge.
Cancer Lifeline
Cancer Lifeline Online Resources
24/7 Helpline: 206.297.2500 or 800.255.5505
Cancer Lifeline is a local cancer organization that provides emotional support, resources, educational classes, artistic expression and exercise support programs for people living with cancer. Patients, survivors, their families, friends, co-workers and caregivers are all welcome. Services are offered free of charge virtually and throughout the Puget Sound area.
View list of Cancer Lifeline's current classes and support programs.
Cancer Pathways
Cancer Pathways offers a broad, community-based program of social, emotional, and educational support for cancer survivors and their loved ones. The program serves everyone touched by cancer across the cancer continuum—from diagnosis, through treatment and post-treatment, survivorship, and bereavement, including children, teens, and entire families.
Cancer Resource Center at Valley
425.690.3507
Friendly volunteers provide the following free services for cancer patients and their loved ones:
- Information on cancer and treatment
- Referrals to and information on local resources, educational programs and support
- Personal Health Manager Kits
- Free wigs, hats and scarves for people experiencing hair loss due to cancer treatment
Caringbridge
CaringBridge.org uses the power of the Internet to bring patients, caregivers, family and friends together to share information and support during life-changing health events such as cancer, premature birth, critical illness and serious accidents. CaringBridge is free and is a meaningful way to help friends and family from around the world stay connected and informed. Patients and caregivers post journal entries about their healthcare journey and in return, family and friends provide vital support through guestbook messages and a photo gallery.
Create your own CaringBridge page today. It’s quick, easy and free. Click here to get started!
Financial Counseling & Assistance
The financial impacts of a cancer diagnosis can be significant. Our team is here to help you navigate the many billing and insurance questions you may have.
In addition, our financial advocates provide financial help and options and can assist with setting up payment plans and evaluating discount, charity care and public assistance options.
CancerCare may offer other financial assistance options.
National Cancer Institute
National Cancer Institute Online Resources
Live Help Instant Online Chat available Monday-Friday, 6AM-6PM PT
NCI Cancer Information Line: 1.800.422.6237 (English and Spanish)
NCI provides comprehensive information about cancer causes and prevention, screening and diagnosis, treatment and survivorship; clinical trials; statistics; and the institute and its programs.
Transportation
Transportation resources to and from medical appointments are available within the community. Please contact the Cancer Resource Center at 425.690.3507 or our Oncology Social Workers for assistance at 425.690.6066.
Additional Online Resources
Bringing HOPE and Support to Valley Cancer Patients
At Valley, we walk beside our patients and their loved ones as they embark on the cancer care journey. The journey is not just a physical one, it is also emotional, mental and tremendously personal for each person it touches. Diagnosis and treatment can be overwhelming and we are dedicated to providing wrap-around support resources that comfort the body, mind and spirit.
 In partnership with Valley Girls & Guys, a local group passionate about being the HOPE for those impacted by cancer, we unite patients, loved ones and caregivers in the quest to provide support and resources for those most in need. Our HOPE Patient Assistance Fund, for example, helps cover living expenses many cancer patients struggle with, like rent or gas to get to treatment. Our acute symptom management program cares for patients undergoing treatment to help keep them out of the ER and healing at home. And our Cancer Resource Cart at Valley has been named after two outstanding Valley Girls & Guys team members – Trapper & Samantha – who were impacted by the care received at Valley and who dedicated their time, creativity and funds to support Valley.
In partnership with Valley Girls & Guys, a local group passionate about being the HOPE for those impacted by cancer, we unite patients, loved ones and caregivers in the quest to provide support and resources for those most in need. Our HOPE Patient Assistance Fund, for example, helps cover living expenses many cancer patients struggle with, like rent or gas to get to treatment. Our acute symptom management program cares for patients undergoing treatment to help keep them out of the ER and healing at home. And our Cancer Resource Cart at Valley has been named after two outstanding Valley Girls & Guys team members – Trapper & Samantha – who were impacted by the care received at Valley and who dedicated their time, creativity and funds to support Valley.
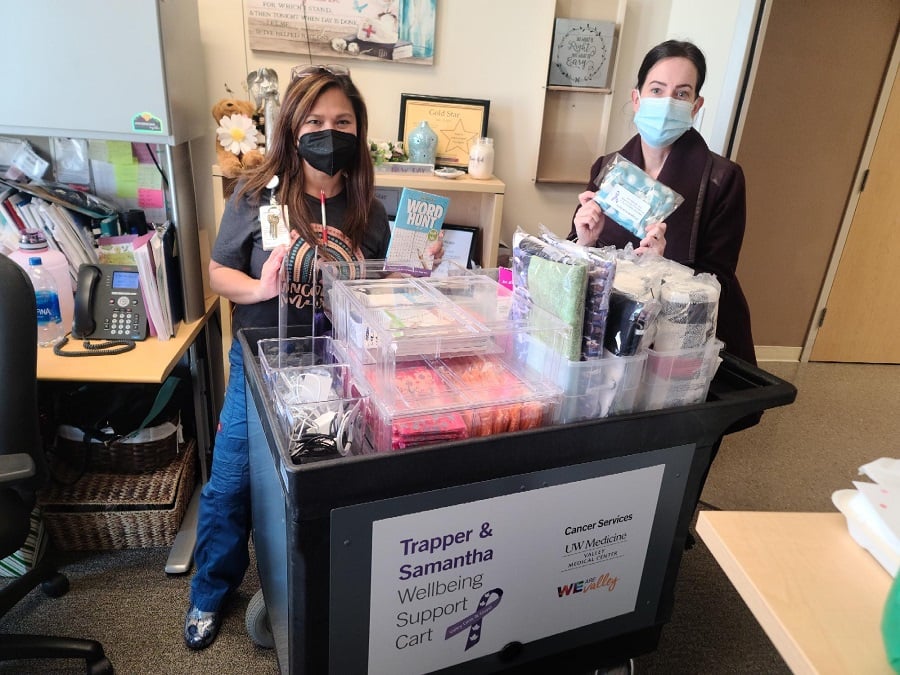 Through the Trapper & Samantha Wellbeing Support Cart, we are able to bring free resources to our cancer patients to help them and their loved ones learn how to live their best lives with cancer. Operated by Valley volunteers, the cart regularly travels through the Infusion Center, providing patients with comfort items and information to make their cancer journey just a bit easier. Whether a handmade hat or a cozy blanket donated by the community, comfy socks, a loaner charging cord, a crossword or sudoku book, comfort items help patients pass the time through their treatment. And information on Valley’s oncology social work team, wig program, transportation resources, and Cancer Lifeline information is also close at hand for patients needing those resources.
Through the Trapper & Samantha Wellbeing Support Cart, we are able to bring free resources to our cancer patients to help them and their loved ones learn how to live their best lives with cancer. Operated by Valley volunteers, the cart regularly travels through the Infusion Center, providing patients with comfort items and information to make their cancer journey just a bit easier. Whether a handmade hat or a cozy blanket donated by the community, comfy socks, a loaner charging cord, a crossword or sudoku book, comfort items help patients pass the time through their treatment. And information on Valley’s oncology social work team, wig program, transportation resources, and Cancer Lifeline information is also close at hand for patients needing those resources.
We are so appreciative of Valley Girls & Guys and Trapper & Samantha for the support, the caring, the love and THE HOPE that you share with us, and through us, with our community. THANK YOU!

NEW Cancer Center - Now Open!
Debbie's Story
This video shares the story of Debbie, a Valley patient. After opting for a home Cologuard test, she received a positive result. Her primary care provider referred her to Joseph Roberts, MD, a gastroenterologist with Valley’s Gastrointestinal Clinic. Dr. Roberts performed her colonoscopy that confirmed she had colon cancer. Colorectal surgeon Greta Bernier, MD, successfully performed a robotic minimally invasive surgery, significantly aiding Debbie’s recovery and return to everyday life. The video highlights Valley’s commitment to patient care, advanced surgical techniques, and the importance of timely cancer screening.
View on our blog.Janette's Story
Janette’s story highlights her cancer care experience at Valley, where she was diagnosed with endometrial cancer after noticing abnormal postmenopausal bleeding. Under the care of Ron Swensen, MD, gynecologic oncologist at Valley’s Oncology & Hematology Clinic, she underwent a minimally-invasive robotic surgery to have a hysterectomy. Grateful for the compassionate care she received, Janette encourages other women to prioritize their health and not hesitate to get health screenings. Her experience motivated her to share her journey in a book, emphasizing the importance of proactive health care.
View on our blog.